Event Volunteer Training
Thank you for supporting GBSI in its goal to promote awareness of group B strep!
On this page you will find:
Please read through the material in each section carefully and take the quizzes to test your knowledge!
On this page you will find:
- General GBS information
- Our statement on membrane stripping
- Info about the US GBS prevention guidelines
- Background information on our organization
Please read through the material in each section carefully and take the quizzes to test your knowledge!
Special note to ACNM volunteers: In speaking with the attendees, please use the word "advocates" instead of "recommends" in regards to what GBSI promotes as we are not a medical governing organization.
Special note to Social Media Intern: Please read GBSI's brochure, status card, and tear sheets for both pregnant women who test positive and for those who test negative for GBS.
General GBS Information
Group B Strep (GBS) is a type of bacteria that is naturally found in the digestive and lower reproductive tracts of both men and women. It is the leading cause of sepsis and meningitis in newborns in the USA and one of the most notable infectious causes of newborn illness and death worldwide. One in 4 women carry GBS. Unfortunately, babies can be infected by GBS before birth and up to about 6 months of age due to their underdeveloped immune systems.
Maternal symptoms and testing
Most women do not show any symptoms; however, GBS can cause vaginal burning/irritation and/or unusual discharge which may be mistaken for a yeast infection and treated incorrectly. It can also cause bladder infections which can be detected through a urine culture (not the standard "dipstick" check). If the urine tests positive, the provider should consider the pregnant woman to be “GBS colonized” for the current pregnancy so she should receive IV antibiotics for GBS when labor starts or her water breaks. GBS is also a transient bacteria which means that a woman could test negative, but be positive later on. In the US, it is standard that pregnant women are tested for GBS at 35-37 weeks during each pregnancy unless their urine already cultured positive in the current pregnancy. The 35-37 week test should be performed by a swab of both the vagina and rectum.
Types of perinatal GBS disease
Prenatal-onset GBS disease (before birth)
Early-onset GBS disease (birth through the first week of life)
Late-onset GBS disease (over 1 week of age through several months of age)
Precautions to help protect babies from infection
During pregnancy:
We advocate a recheck one month after treatment for GBS in urine during pregnancy. People should also be aware that bacteria can be passed between sexual partners, including through oral contact. Providers should tell their patients to contact them immediately for any unexplained fever or decreased/no fetal movement after the 20th week of gestation. Pregnant women should avoid unnecessary, frequent, or forceful internal exams which may push GBS closer to the baby. (Vaginal or perineal ultrasounds are less invasive options). Pregnant women should talk to their providers about not stripping membranes. GBS can cross even intact membranes and procedures such as stripping membranes and using cervical ripening gel to induce labor may push bacteria closer to the baby. Mothers should be aware that, while lower risk, C-sections may not completely prevent GBS infection.
During labor:
Per the CDC guidelines, pregnant women, who do not have a test result, should be offered IV antibiotics based on the following risk factors:
Breastfeeding can supply babies with important antibodies to fight infection; however, it is speculated that a few late-onset and recurrent GBS infections are possibly associated with infected breast milk. It is currently thought though that the health benefits of breastfeeding outweigh any potential risk of exposure to GBS. Health care providers should tell their patients to have everyone wash their hands before handling their baby and make sure everyone who takes care of babies knows the signs of GBS infection in babies and how to respond.
For further information please read our GBS brochure and our All About Group B Strep page
Maternal symptoms and testing
Most women do not show any symptoms; however, GBS can cause vaginal burning/irritation and/or unusual discharge which may be mistaken for a yeast infection and treated incorrectly. It can also cause bladder infections which can be detected through a urine culture (not the standard "dipstick" check). If the urine tests positive, the provider should consider the pregnant woman to be “GBS colonized” for the current pregnancy so she should receive IV antibiotics for GBS when labor starts or her water breaks. GBS is also a transient bacteria which means that a woman could test negative, but be positive later on. In the US, it is standard that pregnant women are tested for GBS at 35-37 weeks during each pregnancy unless their urine already cultured positive in the current pregnancy. The 35-37 week test should be performed by a swab of both the vagina and rectum.
Types of perinatal GBS disease
Prenatal-onset GBS disease (before birth)
Early-onset GBS disease (birth through the first week of life)
Late-onset GBS disease (over 1 week of age through several months of age)
Precautions to help protect babies from infection
During pregnancy:
We advocate a recheck one month after treatment for GBS in urine during pregnancy. People should also be aware that bacteria can be passed between sexual partners, including through oral contact. Providers should tell their patients to contact them immediately for any unexplained fever or decreased/no fetal movement after the 20th week of gestation. Pregnant women should avoid unnecessary, frequent, or forceful internal exams which may push GBS closer to the baby. (Vaginal or perineal ultrasounds are less invasive options). Pregnant women should talk to their providers about not stripping membranes. GBS can cross even intact membranes and procedures such as stripping membranes and using cervical ripening gel to induce labor may push bacteria closer to the baby. Mothers should be aware that, while lower risk, C-sections may not completely prevent GBS infection.
During labor:
Per the CDC guidelines, pregnant women, who do not have a test result, should be offered IV antibiotics based on the following risk factors:
- Her baby will be born before 37 weeks.
- Her water has been broken 18+ hours without delivering. (Even 12+ hours increases the risk.)
- She has a fever of 100.4 °F or higher during labor.
Breastfeeding can supply babies with important antibodies to fight infection; however, it is speculated that a few late-onset and recurrent GBS infections are possibly associated with infected breast milk. It is currently thought though that the health benefits of breastfeeding outweigh any potential risk of exposure to GBS. Health care providers should tell their patients to have everyone wash their hands before handling their baby and make sure everyone who takes care of babies knows the signs of GBS infection in babies and how to respond.
For further information please read our GBS brochure and our All About Group B Strep page
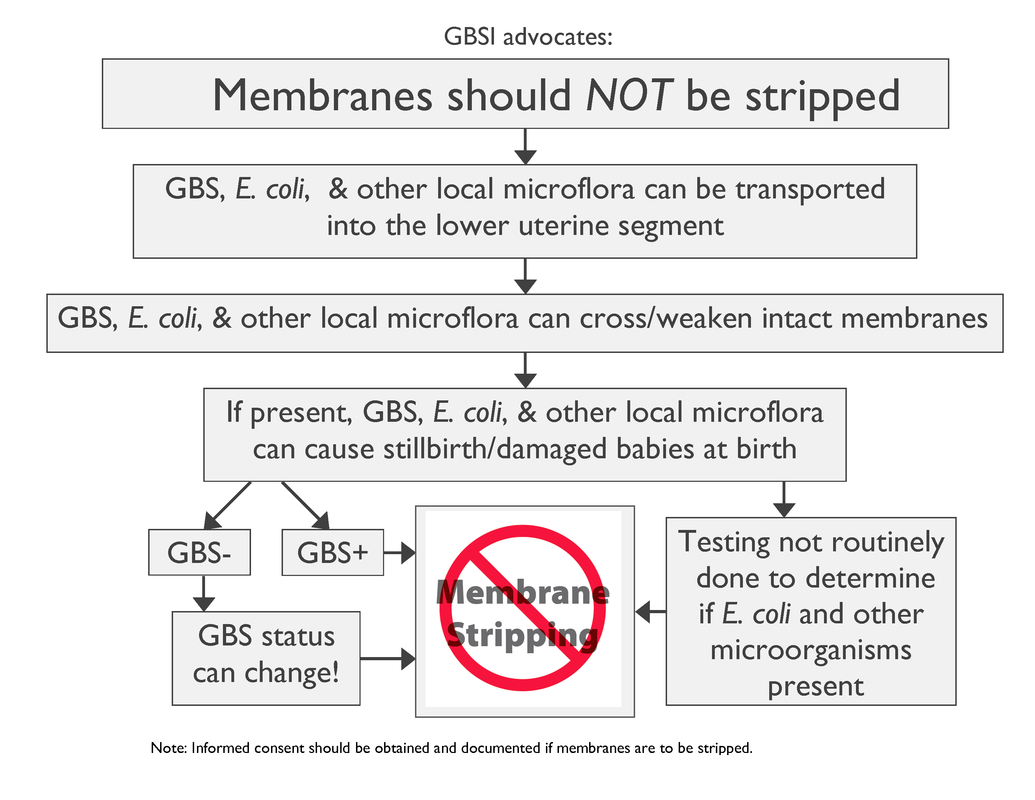
Our Statement on Membrane Stripping
GBSI advocates NO fetal membrane stripping. Fetal membrane stripping (or "sweeping") (FMS) is a "traditional" way to induce labor and delivery. It is widely practiced despite little formal study. The procedure consists of the practitioner forcing their index finger through the cervix and cervical mucous and then forcibly separating the fetal membranes from the uterine lining.
Complications include:
Complications include:
- bleeding
- painful contractions
- intrauterine/perinatal infection
- failure to induce labor or prevent prolonged gestation
- unanticipated pain
Research shows the following:
Membrane stripping is sometimes done without prior patient consent during the course of a routine cervical exam. GBSI advocates that all health care providers do the following prior to this procedure:
- cervical exams can transport microorganisms closer to the baby
- GBS can cross intact membranes
- cervical exams (less invasive than membrane stripping) can increase the risk of perinatal infections
- fetal membrane stripping has not been proven to be safe
- the value of fetal membrane stripping has been repeatedly questioned
Membrane stripping is sometimes done without prior patient consent during the course of a routine cervical exam. GBSI advocates that all health care providers do the following prior to this procedure:
- obtain written informed patient consent
- give a complete explanation of induction and the procedure
- give documented consideration of contraindications as would be required for any medical procedure
GBS Prevention Guidelines and Efforts
|
The CDC issued the most recent guidelines for the Prevention of Perinatal Group B Streptococcal Disease in 2010. (See Figure 1. for the huge decline in early-onset GBS infections due to awareness and prevention efforts in the US.) Please refer people to the guidelines for the answers to any questions you or your team leader can't answer. GBSI supports the CDC guidelines although we advocate against membrane stripping for the above reasons.
|
Background Information on Our Organization
Group B Strep International (GBSI) was formed in April 2006, branching off from its sister organization, The Jesse Cause.
The mission of GBSI is to promote international awareness and prevention of Group B Strep disease in babies before birth through early infancy. Our goal is to be a central resource for GBS information, in a variety of languages, for both the general public and medical professionals. The scope of our mission included actively supporting the GBS awareness and prevention efforts of individuals and organizations on a community or national level.
Health Observance Months sponsored by GBSI:
Social media:
GBSI is a 501(c)(3) nonprofit organization..
For more information on GBSI, please read "GBSI Fast Facts" and learn about Our History and Our Board of Directors.
The mission of GBSI is to promote international awareness and prevention of Group B Strep disease in babies before birth through early infancy. Our goal is to be a central resource for GBS information, in a variety of languages, for both the general public and medical professionals. The scope of our mission included actively supporting the GBS awareness and prevention efforts of individuals and organizations on a community or national level.
Health Observance Months sponsored by GBSI:
- February: International Prenatal Infection Prevention Month
- July: International Group B Strep Awareness Month
- October: Prenatal-onset GBS Disease Recognition Month
Social media:
- Facebook.com/GroupBStrepInternational (FB Page)
- Facebook.com/groups/115986531832/ (FB Groups)
- Twitter.com/GroupBStrep
- YouTube.com/GBSInternational1 (ACNM Volunteers - there are several video testimonials on our YouTube channel from ACNM midwives as to why they don't strip membranes in case that works into your conversations.)
GBSI is a 501(c)(3) nonprofit organization..
For more information on GBSI, please read "GBSI Fast Facts" and learn about Our History and Our Board of Directors.
Thank you for volunteering!