Good morning!
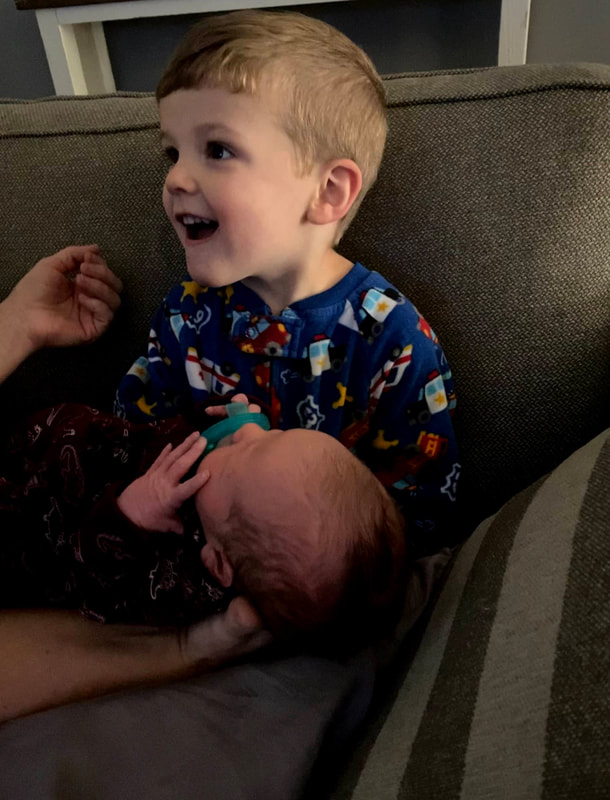
My name is Kelsey Coleman, and I am a 28 year old mother of 2 beautiful boys. My first child, Colt, will be 4 at the end of August and he is a GBS meningitis/sepsis survivor. During my first pregnancy I was employed as a Registered Nurse in Labor and Delivery. As an OB nurse, I had heard of GBS but when mothers asked me about it I normally just told them something like this: “some women carry it in pregnancy and some don’t, it’s not a big deal because if you’re positive we’ll just give you antibiotics and everything will be fine.” I knew that it could be potentially harmful to the baby, but I had never witnessed its effects firsthand. That is, until my own birth experience with Colt.
At my 36 week prenatal appointment a GBS swab was collected and came back as NEGATIVE, therefore I received no antibiotics for GBS prophylaxis during labor. I came in for an induction at 39 weeks gestation. I was admitted at 6:00pm on the night of August 29th 2018, labored through the night, had my bag of water artificially ruptured sometime that next morning, and delivered a seemingly healthy 7 lb 11 oz baby boy at 12:51pm on August 30th 2018. That first afternoon and night were perfect, he was latching well and sleeping well between feedings. We were so thrilled to have him with us finally.
The next day, August 31st 2018, Colt was in the nursery during the morning for his circumcision. He came back to us afterwards and he was beginning to act a little different. Now, being a nurse in this OB unit, I knew baby boys were sometimes more irritable after circumcisions so initially I chalked up his change in behavior to that fact. However, throughout the day he became more irritable, which escalated to him becoming inconsolable. He wouldn’t sleep, wouldn’t nurse, and just kept whimpering. In retrospect, after researching signs and symptoms of GBS infection, I realize now he was grunting and he also appeared mottled. I started to worry by early afternoon, and I asked for our Pediatrician to come see him again. His doctor came back and assessed him again, aside from the “whimpering” he appeared well to him – by this I mean his vital signs were normal and his lungs/heart sounded normal too. We decided to keep watching him and to notify the doctor if anything else changed or any new symptoms developed. I knew, I just knew something was wrong.
Fast forward to around 6:00pm that night (August 31st), when my mother was holding Colt and gently rocking him in an attempt to console him. After a few moments she stopped and began to call his name, unwrap him, and attempted to stimulate him. I started to worry and asked what was wrong, then I asked my mother to hand him back to me. Colt was suddenly very pale, he seemed to of stopped breathing, and he was stiff as a board with his eyes locked upward, almost rolling back in his head. In a panic I grabbed him and ran down the hallway with him because something was clearly wrong. Once I got him into the nursery he had “snapped” out of it. I told them that I believed he had just had a seizure. The nursing staff hooked him up to a cardiopulmonary monitor, but by that time his heartrate and oxygen saturation were back within normal limits. We again called the Pediatrician, who returned to see him and ordered septic lab work and IV antibiotics. Over the next 4 or so hours, we attempted to get an IV placed without any luck. After not nursing (feeding) almost all day, I believe Colt had become somewhat dehydrated and every vein that was stuck for IV placement was blowing. Finally, the Pediatrician himself was able to get an IV placed long enough for Colt to get 1 dose each of two different antibiotics before that IV access infiltrated and had to be removed. Colt’s bloodwork also resulted during this time and his CRP, an inflammatory marker in the blood, was elevated to 11.5. This particular lab can indicate infection and is supposed to be less than 0.2 in otherwise healthy newborns.
Colt remained in the nursery that evening for close monitoring and I began to pump in order to get my milk supply ready for when Colt was able to nurse again. I believe I fell asleep shortly after 1:00am on the morning of September 1st, 2018, then sometime around 2-2:30am our Pediatrician returned to my bedside to inform me that Colt had another “episode, “ which we now know were definitely seizures, and that he needed to be transferred to LeBonheur Children’s Hospital. He had gotten so very sick so very quickly, and I began to sob and ask if he was going to live. My mind rushed to the darkest places and I was so terrified I was going to lose him. Once I was able to calm down enough to breathe normally, I went to the nursery to check on him. Colt was having recurrent seizures, his heartrate would jump to around 170-180 beats per minute and his oxygen saturation would drop into the low 70s. He strained and grunted to breathe with each seizure while I held him and held oxygen up to his nose and mouth trying desperately to increase his oxygen saturation. The flight crew arrived after a few hours and had to place another IV for use in route to LeBonheur. Colt’s bloodwork was repeated just prior to departure and his CRP had almost doubled to 21.7, which is the highest level I have ever seen in a newborn, even to this day I have never seen that again. I loaded Colt into the transport isolette and they took him by helicopter to the NICU in Memphis, TN. I believe he left around 5:30 that morning (September 1st), and we left shortly after to make the 2.5 hour drive to the hospital he was being transported to for NICU services.
The flight crew called us before we could make it to the hospital ourselves and notified us that they had arrived and what room he would be in once we got to the hospital. They told us he did seize again in route and was given medication for it. On arrival, we were taken straight to the NICU to see our boy. Colt was already looking jaundice (yellow) to me at this point and he was lethargic and limp. He had oxygen on via nasal cannula, an umbilical line placed, and a large IV in his bicep. The doctors informed us that he was given a large dose of an anticonvulsant medication and that is the reason he was so lethargic. Honestly, he looked so bad at this point and I was terrified. Sometime that same day, September 1st, no later than noon, we received a call from our delivery hospital. Colt’s blood culture had already began to grow something – group b strep. I was crushed to hear this news, and I didn’t even understand how it was possible because I tested negative. I know now that false negatives for GBS swaps are actually not that uncommon. I was so devastated because he had gotten this from ME, and although everyone tells me it isn’t my fault, I will always feel like it is.
Knowing what they were dealing with now, the doctors changed Colt’s antibiotics to specifically target the GBS bacteria. He had an EEG performed, an MRI, and a lumbar puncture. The MRI showed areas of infarct (damage) from the seizures which had deprived areas of his brain of oxygen. The EEG showed no current seizure activity, and the lumbar puncture confirmed meningitis. He had cerebral swelling as well and remained extremely sedated for the first few days. I continued to pump and they gave him my breastmilk via a nasogastric tube that had been placed shortly after is admission. Also during the first few days, a PICC line was placed for Colt to receive 21 days of penicillin to treat the GBS infection. Colt had just 1 more seizure during the first night of our stay in the NICU and then no more. He was started on Keppra and the more sedative drugs he was receiving were tapered down. I believe it was day 3 or 4 that he finally began to wake up. He was so drowsy and weak initially, but he was able to come off the supplemental oxygen quickly and the umbilical line was removed. We began attempting bottle feeds with a lot of assistance from the nursing staff because he had to relearn how to suck. Once he was taking bottles by mouth, the NG tube was removed.
Over the next 3 weeks Colt was seen by a neonatologist, infectious disease, physical therapy, and neurology teams. He was rounded on by so many teams of doctors each day. His EEG and MRI were repeated during our stay as well. The EEG was normal and the MRI showed the areas of infarct were shrinking but still present. Once I knew he was going to live, I began asking questions about his quality of life. I wanted to know what damage this whole situation inflicted on his poor little body, but because he was so young there was little they could tell me definitely. I wanted to know things like: would he ever walk or talk? The team seeing Colt told us that we wouldn’t know for sure what effects this illness would have on him until he grew and started to potentially miss milestones. They said they were fairly sure he would have difficulties with fine motor skills, but beyond that we would just have to wait and see. The rest of his hospital stay was not without its own obstacles. His PICC line nearly clotted off and had to be adjusted after it migrated too deep into his atria, his TPN infiltrated into his hand, I developed mastitis, and they were concerned he was developing osteomyelitis. However, despite all that, after 21 long days we were discharged home with our boy. He was sent home on Keppra to hopefully prevent anymore seizures and set to follow-up with our Pediatrician that next week.
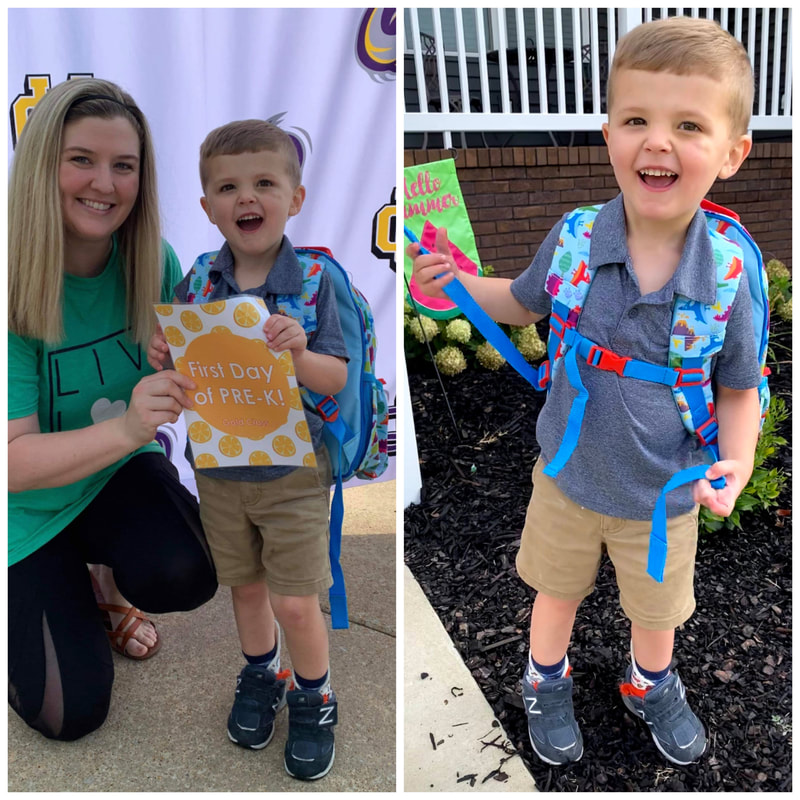
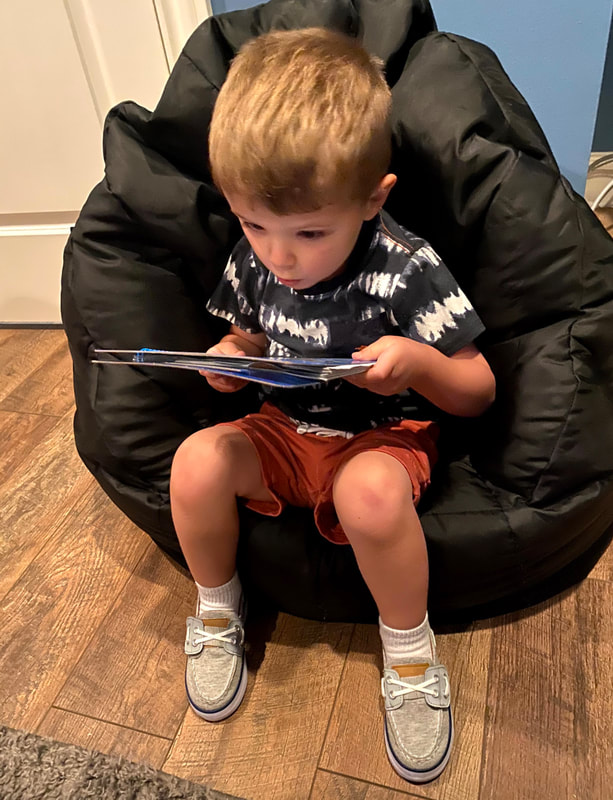
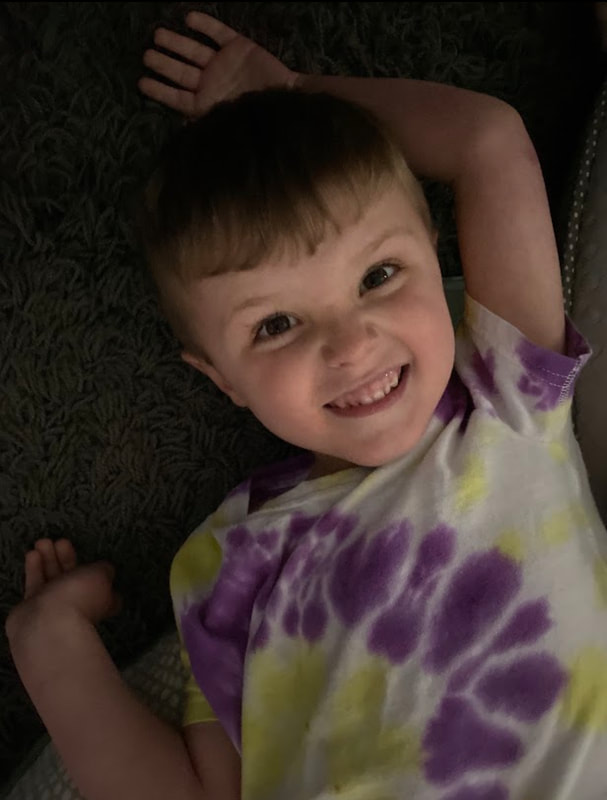
Over the next 2 years we would take him back and forth for audiology, neurology, and developmental follow-up appointments at LeBonheur. Meningitis can cause delayed hearing loss so his hearing would be closely monitored every 3-6 months until he turned 3 years old. Thankfully, we have not had any issues with hearing. By 9 months, Colt was evaluated by PT and OT specialists, and by just over a year old he was also evaluated by speech therapy. At 1 year old, Colt was not crawling or walking so he started physical therapy. He did start walking around 14-15 months with regular physical therapy appointments and ankle braces to assist with his strength/balance. He continues to do OT and speech weekly to this day. He will be 4 years old on August 30th of this year, and he is less coordinated than his classmates, especially with eating and writing utensils. We see his struggles with fine motor skills mostly and definitely in his delayed speech. He has been diagnosed with a developmental delay as well, and it is hard to fully assess what he does and does not know since he is mostly non-verbal. Our therapists are wonderful and I am eager to hear him speak. He’s so smart and he works so hard at therapy. I have confidence we can get him caught up, and even if we don’t, he is the most wonderful child. Colt is healthy, happy, and hilarious – he has the BEST personality and he is our miracle. I am so thankful he’s here with us today, and although I will never stop beating myself up over what happened, I am so proud of how far he has come. We’ve been working on sign language cues and he also has a communication tablet, so one way or another he’ll find a way to communicate with us and we’ll continue advocating for him to get any/all treatments and evaluations he may need.
Since 2018, I have researched a lot about GBS infection and always heavily advocate for mother’s to make sure they get the necessary testing and treatment. One in 4 pregnant women carry GBS – ONE in FOUR! It can harm babies in utero, at birth, and for months after birth. It is the leading case of neonatal meningitis and one of the leading causes of both neonatal and maternal deaths. Educate yourselves, know what to look for, and advocate for your child!! If you feel it in your gut that something is wrong, fight to get it taken care of because a mother knows! We just do, it’s in our biology. I pray that treatment becomes universal one day or testing becomes more accurate. I’ve even seen research mentioning a GBS vaccine. I don’t wish this horrific experience on anyone and it could have ended so much worse for us. With my next pregnancy I received more than ample treatment for GBS and my second son was delivered via c-section as well. That pregnancy provoked a lot of anxiety in me as well, I was so scared something like this would happen again. Thankfully we have 2 amazing little boys at home today – a 1 year old and nearly 4 year old. I will continue to tell Colt’s story until my last breath and hope it helps spread awareness on this issue! God bless you.
- Kelsey C
Kelsey shares information with others by talking to patients about it since she's a labor and delivery nurse
My name is Kelsey Coleman, and I am a 28 year old mother of 2 beautiful boys. My first child, Colt, will be 4 at the end of August and he is a GBS meningitis/sepsis survivor. During my first pregnancy I was employed as a Registered Nurse in Labor and Delivery. As an OB nurse, I had heard of GBS but when mothers asked me about it I normally just told them something like this: “some women carry it in pregnancy and some don’t, it’s not a big deal because if you’re positive we’ll just give you antibiotics and everything will be fine.” I knew that it could be potentially harmful to the baby, but I had never witnessed its effects firsthand. That is, until my own birth experience with Colt.
At my 36 week prenatal appointment a GBS swab was collected and came back as NEGATIVE, therefore I received no antibiotics for GBS prophylaxis during labor. I came in for an induction at 39 weeks gestation. I was admitted at 6:00pm on the night of August 29th 2018, labored through the night, had my bag of water artificially ruptured sometime that next morning, and delivered a seemingly healthy 7 lb 11 oz baby boy at 12:51pm on August 30th 2018. That first afternoon and night were perfect, he was latching well and sleeping well between feedings. We were so thrilled to have him with us finally.
The next day, August 31st 2018, Colt was in the nursery during the morning for his circumcision. He came back to us afterwards and he was beginning to act a little different. Now, being a nurse in this OB unit, I knew baby boys were sometimes more irritable after circumcisions so initially I chalked up his change in behavior to that fact. However, throughout the day he became more irritable, which escalated to him becoming inconsolable. He wouldn’t sleep, wouldn’t nurse, and just kept whimpering. In retrospect, after researching signs and symptoms of GBS infection, I realize now he was grunting and he also appeared mottled. I started to worry by early afternoon, and I asked for our Pediatrician to come see him again. His doctor came back and assessed him again, aside from the “whimpering” he appeared well to him – by this I mean his vital signs were normal and his lungs/heart sounded normal too. We decided to keep watching him and to notify the doctor if anything else changed or any new symptoms developed. I knew, I just knew something was wrong.
Fast forward to around 6:00pm that night (August 31st), when my mother was holding Colt and gently rocking him in an attempt to console him. After a few moments she stopped and began to call his name, unwrap him, and attempted to stimulate him. I started to worry and asked what was wrong, then I asked my mother to hand him back to me. Colt was suddenly very pale, he seemed to of stopped breathing, and he was stiff as a board with his eyes locked upward, almost rolling back in his head. In a panic I grabbed him and ran down the hallway with him because something was clearly wrong. Once I got him into the nursery he had “snapped” out of it. I told them that I believed he had just had a seizure. The nursing staff hooked him up to a cardiopulmonary monitor, but by that time his heartrate and oxygen saturation were back within normal limits. We again called the Pediatrician, who returned to see him and ordered septic lab work and IV antibiotics. Over the next 4 or so hours, we attempted to get an IV placed without any luck. After not nursing (feeding) almost all day, I believe Colt had become somewhat dehydrated and every vein that was stuck for IV placement was blowing. Finally, the Pediatrician himself was able to get an IV placed long enough for Colt to get 1 dose each of two different antibiotics before that IV access infiltrated and had to be removed. Colt’s bloodwork also resulted during this time and his CRP, an inflammatory marker in the blood, was elevated to 11.5. This particular lab can indicate infection and is supposed to be less than 0.2 in otherwise healthy newborns.
Colt remained in the nursery that evening for close monitoring and I began to pump in order to get my milk supply ready for when Colt was able to nurse again. I believe I fell asleep shortly after 1:00am on the morning of September 1st, 2018, then sometime around 2-2:30am our Pediatrician returned to my bedside to inform me that Colt had another “episode, “ which we now know were definitely seizures, and that he needed to be transferred to LeBonheur Children’s Hospital. He had gotten so very sick so very quickly, and I began to sob and ask if he was going to live. My mind rushed to the darkest places and I was so terrified I was going to lose him. Once I was able to calm down enough to breathe normally, I went to the nursery to check on him. Colt was having recurrent seizures, his heartrate would jump to around 170-180 beats per minute and his oxygen saturation would drop into the low 70s. He strained and grunted to breathe with each seizure while I held him and held oxygen up to his nose and mouth trying desperately to increase his oxygen saturation. The flight crew arrived after a few hours and had to place another IV for use in route to LeBonheur. Colt’s bloodwork was repeated just prior to departure and his CRP had almost doubled to 21.7, which is the highest level I have ever seen in a newborn, even to this day I have never seen that again. I loaded Colt into the transport isolette and they took him by helicopter to the NICU in Memphis, TN. I believe he left around 5:30 that morning (September 1st), and we left shortly after to make the 2.5 hour drive to the hospital he was being transported to for NICU services.
The flight crew called us before we could make it to the hospital ourselves and notified us that they had arrived and what room he would be in once we got to the hospital. They told us he did seize again in route and was given medication for it. On arrival, we were taken straight to the NICU to see our boy. Colt was already looking jaundice (yellow) to me at this point and he was lethargic and limp. He had oxygen on via nasal cannula, an umbilical line placed, and a large IV in his bicep. The doctors informed us that he was given a large dose of an anticonvulsant medication and that is the reason he was so lethargic. Honestly, he looked so bad at this point and I was terrified. Sometime that same day, September 1st, no later than noon, we received a call from our delivery hospital. Colt’s blood culture had already began to grow something – group b strep. I was crushed to hear this news, and I didn’t even understand how it was possible because I tested negative. I know now that false negatives for GBS swaps are actually not that uncommon. I was so devastated because he had gotten this from ME, and although everyone tells me it isn’t my fault, I will always feel like it is.
Knowing what they were dealing with now, the doctors changed Colt’s antibiotics to specifically target the GBS bacteria. He had an EEG performed, an MRI, and a lumbar puncture. The MRI showed areas of infarct (damage) from the seizures which had deprived areas of his brain of oxygen. The EEG showed no current seizure activity, and the lumbar puncture confirmed meningitis. He had cerebral swelling as well and remained extremely sedated for the first few days. I continued to pump and they gave him my breastmilk via a nasogastric tube that had been placed shortly after is admission. Also during the first few days, a PICC line was placed for Colt to receive 21 days of penicillin to treat the GBS infection. Colt had just 1 more seizure during the first night of our stay in the NICU and then no more. He was started on Keppra and the more sedative drugs he was receiving were tapered down. I believe it was day 3 or 4 that he finally began to wake up. He was so drowsy and weak initially, but he was able to come off the supplemental oxygen quickly and the umbilical line was removed. We began attempting bottle feeds with a lot of assistance from the nursing staff because he had to relearn how to suck. Once he was taking bottles by mouth, the NG tube was removed.
Over the next 3 weeks Colt was seen by a neonatologist, infectious disease, physical therapy, and neurology teams. He was rounded on by so many teams of doctors each day. His EEG and MRI were repeated during our stay as well. The EEG was normal and the MRI showed the areas of infarct were shrinking but still present. Once I knew he was going to live, I began asking questions about his quality of life. I wanted to know what damage this whole situation inflicted on his poor little body, but because he was so young there was little they could tell me definitely. I wanted to know things like: would he ever walk or talk? The team seeing Colt told us that we wouldn’t know for sure what effects this illness would have on him until he grew and started to potentially miss milestones. They said they were fairly sure he would have difficulties with fine motor skills, but beyond that we would just have to wait and see. The rest of his hospital stay was not without its own obstacles. His PICC line nearly clotted off and had to be adjusted after it migrated too deep into his atria, his TPN infiltrated into his hand, I developed mastitis, and they were concerned he was developing osteomyelitis. However, despite all that, after 21 long days we were discharged home with our boy. He was sent home on Keppra to hopefully prevent anymore seizures and set to follow-up with our Pediatrician that next week.
Over the next 2 years we would take him back and forth for audiology, neurology, and developmental follow-up appointments at LeBonheur. Meningitis can cause delayed hearing loss so his hearing would be closely monitored every 3-6 months until he turned 3 years old. Thankfully, we have not had any issues with hearing. By 9 months, Colt was evaluated by PT and OT specialists, and by just over a year old he was also evaluated by speech therapy. At 1 year old, Colt was not crawling or walking so he started physical therapy. He did start walking around 14-15 months with regular physical therapy appointments and ankle braces to assist with his strength/balance. He continues to do OT and speech weekly to this day. He will be 4 years old on August 30th of this year, and he is less coordinated than his classmates, especially with eating and writing utensils. We see his struggles with fine motor skills mostly and definitely in his delayed speech. He has been diagnosed with a developmental delay as well, and it is hard to fully assess what he does and does not know since he is mostly non-verbal. Our therapists are wonderful and I am eager to hear him speak. He’s so smart and he works so hard at therapy. I have confidence we can get him caught up, and even if we don’t, he is the most wonderful child. Colt is healthy, happy, and hilarious – he has the BEST personality and he is our miracle. I am so thankful he’s here with us today, and although I will never stop beating myself up over what happened, I am so proud of how far he has come. We’ve been working on sign language cues and he also has a communication tablet, so one way or another he’ll find a way to communicate with us and we’ll continue advocating for him to get any/all treatments and evaluations he may need.
Since 2018, I have researched a lot about GBS infection and always heavily advocate for mother’s to make sure they get the necessary testing and treatment. One in 4 pregnant women carry GBS – ONE in FOUR! It can harm babies in utero, at birth, and for months after birth. It is the leading case of neonatal meningitis and one of the leading causes of both neonatal and maternal deaths. Educate yourselves, know what to look for, and advocate for your child!! If you feel it in your gut that something is wrong, fight to get it taken care of because a mother knows! We just do, it’s in our biology. I pray that treatment becomes universal one day or testing becomes more accurate. I’ve even seen research mentioning a GBS vaccine. I don’t wish this horrific experience on anyone and it could have ended so much worse for us. With my next pregnancy I received more than ample treatment for GBS and my second son was delivered via c-section as well. That pregnancy provoked a lot of anxiety in me as well, I was so scared something like this would happen again. Thankfully we have 2 amazing little boys at home today – a 1 year old and nearly 4 year old. I will continue to tell Colt’s story until my last breath and hope it helps spread awareness on this issue! God bless you.
- Kelsey C
Kelsey shares information with others by talking to patients about it since she's a labor and delivery nurse
|
Dear Scientist, Group B Streptococcus severely impacted my son’s development. Can prevention for newborns be improved? | Full Article
“Even if one person would benefit from it, it would definitely be worth it because I would never want what happened with our son to happen to anybody else’s child,” Kelsey says. “It’s comforting to know that there are people out there striving to make sure that it doesn’t.” |
The last six photos are just a few of my favorites from Colt’s third year of life. He’s an amazing little boy with a big personality. He’ll be 4 this year and he continues to receive both occupational and speech therapies each week. He’s a SURVIVOR and we are beyond blessed that God chose us to be his parents. I hope his story gives someone comfort that is facing any of the same struggles and brings awareness to the issue of Group B Strep colonization in pregnancy.
To learn more about Perinatal & GBS Misconceptions, click HERE.
To learn more about the Signs & Symptoms of Preterm Labor, click HERE.
To learn more about the Signs & Symptoms of GBS Infection, click HERE.
To learn more about Why Membranes Should NOT Be Stripped, click HERE.
To learn more about How to Help Protect Your Baby from Group B Strep (GBS), click HERE.
To learn more about the Signs & Symptoms of Preterm Labor, click HERE.
To learn more about the Signs & Symptoms of GBS Infection, click HERE.
To learn more about Why Membranes Should NOT Be Stripped, click HERE.
To learn more about How to Help Protect Your Baby from Group B Strep (GBS), click HERE.